How Dual Diagnosis Impacts Recovery in Massachusetts
Are you wondering how facing two battles at once can shape the path to healing? “Recovery is an acceptance that your life is in shambles, and you have to change,” says James Lee Curtis—words that echo in every dual diagnosis journey.
In Massachusetts, more than 50% of those seeking substance abuse treatment also struggle with mental health conditions. This intertwining adds layers of complexity to the recovery process, but it also reveals new paths forward.
Discover how understanding this challenge can unlock true hope—and why this article holds the insights that could change everything for you or someone you love.
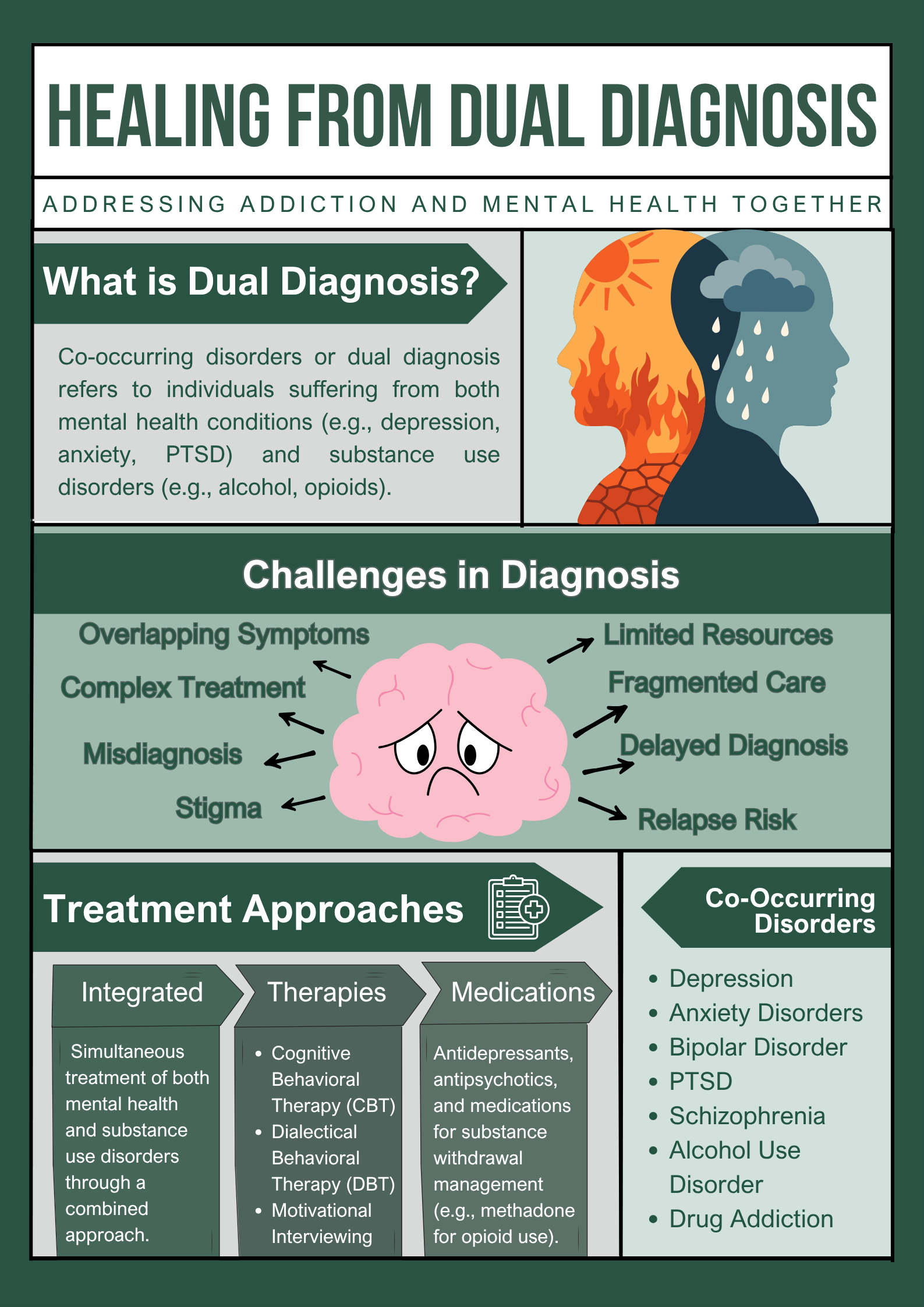
Understanding Dual Diagnosis in Massachusetts
What happens when mental health struggles and addiction collide? In Massachusetts, dual diagnosis—facing both conditions together—affects one out of every two people living with severe mental illness. That’s over 200,000 adults statewide, wrestling with overlapping challenges.
Breaking Down the Issue
- Depression is often linked with alcohol issues
- Anxiety frequently pairs with opioid misuse
- PTSD raises risk for substance use
What Makes It Tough Locally
Urban stress in Boston boosts cases. Rural areas miss quick help. The opioid crisis killed over 80,000 people in 2023, which is 76% of total deaths from drug use. Many are linked to ignored mental ills. Clover Behavioral Health spots this often. We untangle with early screens.
- Key Combos: Depression + alcohol; anxiety + opioids.
- Daily Struggles: Work slips, home life frays without aid.
- Hope Factor: Integrated care treats both, cuts stigma, and rebuilds hope.
Massachusetts needs better access, as education helps families spot signs fast. Outcomes improve with timely care, and people regain control.
Why Dual Diagnosis Makes Recovery More Complex
Dual diagnosis twists recovery paths in tricky ways. Mental health symptoms can spark cravings. Addiction clouds clear thinking. In Massachusetts, cold winters worsen depression. That pushes some to self-medicate with drugs.
Relapse rates climb to 60% without dual care. Misdiagnosis happens often. Doctors might treat only addiction first. But anxiety or bipolar disorder hides underneath. This cycle drains energy. Relationships suffer too. Jobs get lost.
Clover Behavioral Health knows this well. We use therapies that address both. Patients build skills to break the loop.
Complexity comes from denial, too. Many ignore mental health needs and focus on quitting substances alone. But that fails without full support. In Massachusetts, stigma stops people from seeking help. Cultural views also play a role.
Co-occurring disorders need tailored plans, as therapy plus medication works best in such cases. Support groups help share stories and provide a platform for you to relate to people facing similar struggles.
That’s why Clover Behavioral Health offers group sessions weekly to build a sense of community. So, the recovery feels less lonely. Facts also support the notion that integrated treatment reduces relapse by 40%, which is significant for long-term success.
Substance Abuse Trends and Mental Health in Massachusetts
Substance abuse in Massachusetts often ties right into mental health struggles. Opioids still lead the pack, but good news—overdose deaths dropped 36% to 1,763 in 2024. Fentanyl fuels many of those. Alcohol abuse trails close.
Roughly 50,000 adults are involved in binge drinking and alcohol abuse, which spikes anxiety levels. Cocaine and other stimulants surge in cities. They poorly hide ADHD issues. Dual diagnosis mixes these up badly.
Clover Behavioral Health monitors this closely and tweaks programs to fit. As risk education really saves lives.
Gaps in Mental Health Trends
Suicide rates rose 10% last year, and the majority of cases involved substance abuse. Bipolar often pairs with meth, and Schizophrenia links to cannabis misuse. Economic stress in Worcester fuels this even more. Job loss triggers worsen such episodes.
While recovery requires sharp awareness, Clover Behavioral Health takes note of this data to provide optimal care, enabling patients to identify patterns and initiate prevention measures early.
Moreover, Schools are also teaching coping strategies now to minimize future risks.
Key Insights on Trends
- Opioid Shift: Deaths fell sharply, but fentanyl remains in 92% of cases.
- Alcohol Impact: Over 50,000 ER visits yearly are tied to bingeing.
- Mental Ties: 37% of abusers battle serious illness, per state reports.
Unique Barriers to Treatment in Massachusetts
Getting help for dual diagnosis isn’t simple in Massachusetts. Between insurance limits and long waitlists, many people fall through the cracks.
Major Barriers to Treatment
- Insurance coverage for dual diagnosis is inconsistent. Some plans cut the number of allowed therapy sessions.
- Rural communities (like the Berkshires) have too few clinics, while city clinics are overloaded.
- Wait times for state treatment programs can run months.
- Language differences block care for many, especially in immigrant families.
- COVID-19 shrank clinical staffing and slowed program intakes.
Where Can You Get Real Help?
Clover Behavioral Health bridges these gaps:
- Offers telehealth for remote patients.
- Uses sliding-scale fees.
- Partners with transport services.
- Early education campaigns make seeking care easier.
About 40% of patients drop out mainly due to these barriers. Consistent state efforts and integrated programs are necessary to enhance access and improve success rates.
|
Barrier |
Impact |
Clover Solution |
|
Insurance Limits |
Delays care |
Sliding-scale payments |
|
Waitlists |
Increases relapse |
Priority screenings |
|
Rural Access |
Isolation grows |
Telehealth sessions |
Effective Recovery Strategies for Dual Diagnosis
Tackling dual diagnosis recovery starts with the basics that stick. In Massachusetts, simple steps like daily stress management can transform lives.
Everyday Tools
- Build routines with good sleep and balanced meals to help cut cravings fast.
- Nature walks in state parks are also beneficial.
- Journal writing can help to spot triggers.
- Clover Behavioural Health teaches these skills during treatment to facilitate effective recovery.
Advanced Moves
Mix therapies like CBT and DBT with meds. Set weekly goals. Track progress. Avoid old spots. Pick up hobbies or volunteer. Workshops build purpose. Exercise slashes symptoms by 30%.
- Mindfulness Daily: Breathe deep to stay calm.
- Support Groups: Join local ones for motivation.
- Mood Tracking: Use journals to see patterns.
With these steps, recovery becomes possible, and the risk of relapse decreases over time.

Support for Families in Massachusetts
Family support is at the heart of dual diagnosis recovery. When loved ones are involved, hope and healing grow stronger in Massachusetts.
Why Family Matters
- Groups like NAMI and Al-Anon meet statewide, offering tools and comfort.
- Clover Behavioural Health hosts family nights, teaching effective communication skills.
- Setting healthy boundaries—like avoiding enabling actions—protects everyone.
- Caregivers need breaks, their own therapy, and advice from support hotlines.
Learning about co-occurring disorders and recognizing relapse signs prepares families for tough times. Research shows that families who get support see up to 50% better recovery outcomes. Connection creates progress.
Real-World Dual Diagnosis Recovery: A Massachusetts Story
Mike is a 35-year-old veteran from Boston battling PTSD and opioid addiction. He hit rock bottom after years of self-medicating nightmares with pills. At Evoke Wellness in Cohasset, integrated care changed everything.
Therapists used CBT to unpack trauma, while meds eased cravings. Group sessions built his support circle. Six months in, Mike’s clean and managing anxiety—back at work, even coaching youth sports. It’s proof that dual diagnosis treatment works when both issues are tackled together.
- Key Wins: Reduced relapse by 50% through combined therapy.
- Challenges Overcome: Broke the self-medication cycle with holistic plans.
- Long-Term Tip: Ongoing alumni groups keep motivation high.
Massachusetts Resources and Helplines
|
Resource |
Contact |
Focus |
|
Mass Helpline |
1-800-327-5050 |
General crisis |
|
NAMI MA |
Online groups |
Mental health support |
|
SAMHSA |
Locator tool |
Treatment finder |
|
Veterans Line |
1-877-424-3838 |
Veteran support |
|
Crisis Text |
Text 741741 |
Immediate help |

Taking the First Step—Getting Help in Massachusetts
Ready to take the next step toward true recovery? Massachusetts faces tough odds, but you aren’t alone. If dual diagnosis has complicated your journey or a loved one’s life, it’s time for a change.
With resources, support, and expert care like Clover Behavioral Health provides, hope is within reach. Why wait for things to get worse? Every day, real people overcome these hurdles—and you can too.
Call for help, join a group, and let brighter days begin now. Isn’t a better future worth fighting for? Empower yourself today—let your next chapter start strong.