From Burnout to Balance: Why a Resident Chose an Intensive Outpatient Program Near Keene, NH
For a long time, Walt didn’t think an intensive outpatient program was meant for him.
He wasn’t in crisis! He was still working and showing up for family and responsibilities. Life looked fine from the outside, even if it felt exhausting on the inside.
When Walt first heard about an intensive outpatient program near Keene, NH, he thought what most people usually think, “That’s for people who are worse off than me!”
This is a case study based on real experiences. It shows that the decision to enter an IOP is not from hitting rock bottom but from realizing that trying to keep going on your own isn’t working anymore.
In Denial That Anything Was Wrong
Walt had learned how to function under pressure. Stress had been part of life for years, and like many adults, he adapted by pushing harder. Deadlines were met, obligations were handled, and breaks? Well, they were always postponed!
Over time, the strain started showing up in quieter ways.
- Sleep became inconsistent
- Concentration slipped
- Small problems felt heavier than they used to
- Emotional reactions felt sharper and harder to control
Still, Walt told himself the same thing, “This is just life right now.”
Why Weekly Therapy Didn’t Feel Like Enough?
Walt had already taken a step toward support by starting weekly therapy. The sessions helped make sense of what was happening emotionally, but something still felt off.
Between appointments, stress built quickly. Coping tools made sense during therapy, but it was hard to use them in everyday life situations. By the time the next session arrived, Walt often felt like he was starting over.
The problem wasn’t therapy, it was the week-long gap!
That’s when the idea of needing more support via an intensive outpatient program near Keene, NH, first surfaced.
The Misconceptions About IOP That Got in the Way
Even as the idea lingered, Walt resisted it. He imagined IOP as:
- Too intense
- Too disruptive
- Something that would take over his life
- A sign that he was doing worse than he wanted to admit
There was also a deeper fear underneath it all: “What if IOP means I can’t keep up with work or responsibilities?”
So Walt kept going as he was, hoping things would stabilize on their own.
They didn’t!
The Question That Changed Everything
The change didn’t happen because of a big event or a crisis. It happened when Walt realized how much effort it took just to keep going.
- Workdays felt draining before they even started.
- Decision-making felt heavier.
- Rest didn’t restore anything anymore.
The idea of continuing like this indefinitely felt unsettling.
Instead of asking, “Am I bad enough for IOP?” Walt found himself asking, “Why am I waiting to feel worse before getting more support?”
That question changed everything!
Learning What IOP Actually Is and Isn’t
When Walt finally explored an intensive outpatient program near Keene, NH, the reality was very different from what he had imagined.
IOP wasn’t about stepping away from life; it was about adding structure to life.
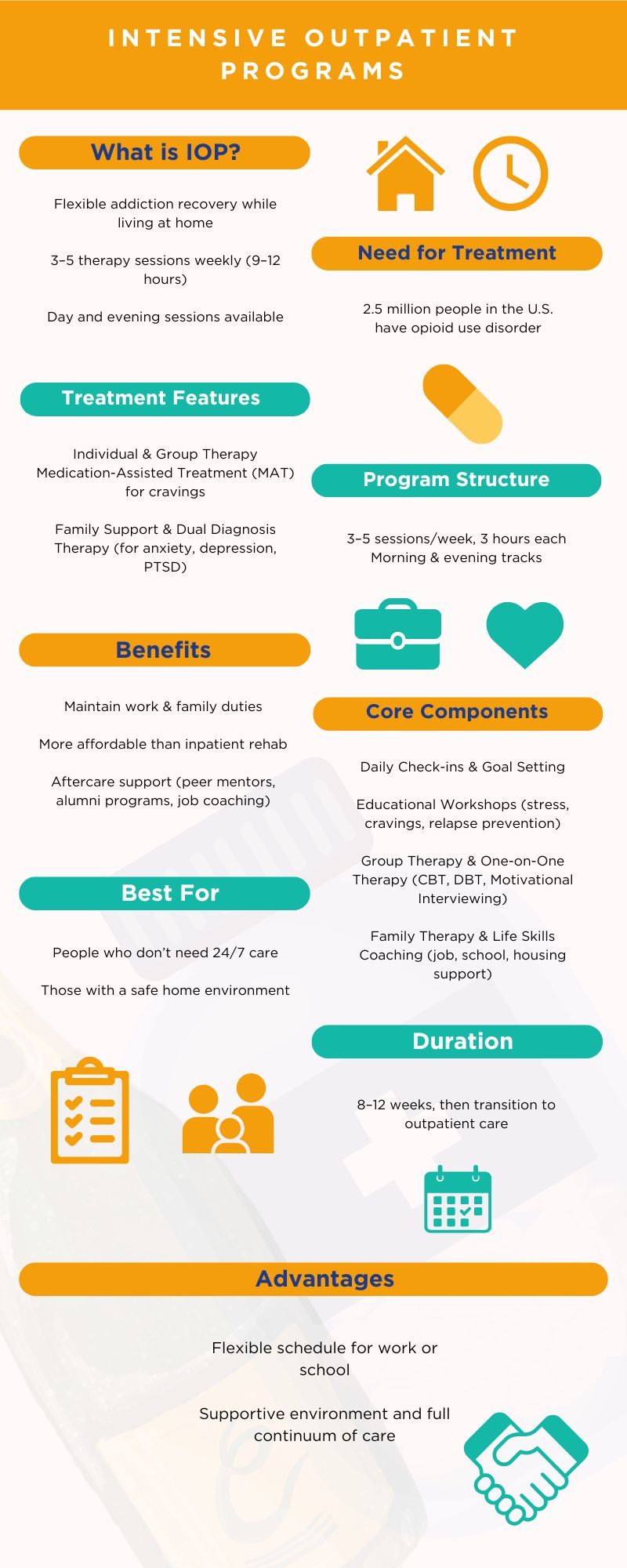
He learned that IOP typically involves:
- Multiple sessions per week
- A predictable schedule
- More consistent support than weekly therapy
- The ability to keep working and living at home
Reaching Out to Clover Behavioral Health
Walt’s first conversation with our licensed therapist at Clover Behavioral Health felt unexpectedly grounding.
Instead of being told what he needed, Walt was asked thoughtful questions:
- What feels hardest right now?
- What has been working, and what hasn’t?
- What does a typical week look like?
Walt discussed with his therapist whether an intensive outpatient program was a helpful support option, rather than just a label.
Why the Decision Finally Felt Right?
What helped Walt make an informed decision wasn’t pressure; it was clarity.
The IOP at Clover BH offered:
- More frequent support during the week
- Accountability without judgment
- Space to practice coping skills while still living real life
- A way to address stress before it turns into something bigger
What Changed Because of the Choice?
The biggest shift due to IOP was steadiness, not immediate relief.
Having consistent sessions throughout the week created a routine that Walt hadn’t realized he was missing. It didn’t make the stress disappear; however, it didn’t pile up the same way.
Instead of holding everything in until it overflowed, there was a regular place to vent about what was happening.
Over time, Walt noticed:
- Better emotional regulation
- Improved focus at work
- More awareness of stress signals
- Less reactivity and more pause
These weren’t dramatic changes; they were meaningful ones.
Why Structure Helped More Than Time Off?
One of Walt’s biggest surprises was realizing that structure, not rest alone, was what he needed.
Time off had always been temporary. The same stress returned as soon as his routine resumed. IOP, on the other hand, helped Walt change how he responded to stress inside those routines.
How Clover Behavioral Health Approaches IOP?
At Clover Behavioral Health, our intensive outpatient program helps people who are managing daily life but feel overwhelmed. We focus on providing consistent support, offering practical coping strategies, and helping clients recognize their stress patterns before they worsen.
The goal isn’t to take over someone’s life, but to support it.
Final Thoughts
Many people wait to feel bad enough before seeking more help. Walt’s story shows another option: choosing support when life feels unsustainable, even if it still looks fine on the outside.
If you’re considering an intensive outpatient program near Keene, NH, it doesn’t mean you’ve failed or fallen behind. It may simply mean you’re ready to stop carrying everything alone.
At Clover Behavioral Health, we offer IOP designed to fit real lives and real responsibilities.
So, take the first step and reach out today! There’s no harm in getting information that helps you make the right choice!