The Five Essential Components of Mental Health Evaluation in Westford, MA
One in five adults in Massachusetts experiences a mental health condition each year. Let that sink in. One in five. Look around your neighborhood in Westford. Count five houses. One of them is fighting a battle most people never talk about.
Why, then, do 60 percent of those people never seek help?
Think about that point in Inside Out when Riley eventually loses it and admits that she is not okay? She has been attempting to make herself happy the entire movie, faking that everything is going well when her world is collapsing around her. Then she stops running. Stop pretending. And let someone see the truth.
That’s what a mental health evaluation is. The moment you stop performing and let someone look.
Nobody ever tells you, however, that there is a system involved. Five crucial elements that combine and collaborate to determine what the real picture really is. Not guesswork. Not a casual chat. A comprehensive assessment that takes your chaos and turns it into something we can actually work with.
This is what happens when you walk through that door in Westford.
1. Patient History: The Part Where Your Past Gets a Voice
You know how sometimes you meet someone, and within five minutes they’re telling you their whole life story? Patient history is the clinical version of that. Except it matters more. A lot more.
Your clinician wants to know when things started falling apart. Was it gradual, like sand through fingers? Or sudden, like a door slamming? They are not nosy when they ask about your childhood, but the brain you brought to this appointment was a result of all that came before.
They’ll ask about your family. Not the holiday card version. The real one. Depression runs in families like brown eyes do. So does anxiety. Addiction. Trauma.
Medical history comes up too. That thyroid medication you’ve been on for years? Your brain doesn’t exist separate from your body. When something’s off physically, it shows up mentally.
Indeed, they will inquire about drugs. They’re not passing judgment. Rather, alcohol and drugs rewrite brain chemistry, and they need to know what they’re working with.
People sometimes lie in this part. Or minimize. “I have a few drinks” when they mean “I finish a bottle most nights.” The truth is, though, your clinician has heard everything. They just need the truth to help you.
2. Mental Status Examination: What You Don’t Know You’re Showing
This part happens whether you know it’s happening or not.
From the moment you walk in, your clinician is observing. They’re noticing how you’re dressed. Not judging your style. Checking if you seem to be taking care of yourself. Sometimes depression shows up first in unwashed hair and mismatched socks.
Your speech matters. Are you talking so fast that the words trip over each other? Are the sentences coming out slow and heavy, like each word costs something? They’re also watching your mood. What you say you’re feeling versus what your face is doing. Sometimes those don’t match. That gap matters.
This examination isn’t a test you can fail. It’s a snapshot. This is what your mental state looks like on this day, at this moment, in this room.
3. Psychological Testing: When Numbers Tell Stories Words Can’t
Most people hear “testing” and think pop quiz. Stress. Performance. Pass or fail.
Psychological testing isn’t that. It’s more like someone’s trying to measure something invisible. Your depression. Your anxiety. Your trauma. These things don’t show up on X-rays. So we use questionnaires that have been refined over decades to catch what’s hiding.
Sometimes it’s a simple screening. PHQ-9 for depression. GAD-7 for anxiety. You circle numbers that correspond to how often you feel certain ways. Your answers create a score. The score creates a picture.
Other times, testing goes deeper. Personality assessments. Cognitive functioning tests. Tools that help figure out if there’s ADHD hiding under the anxiety or if trauma is masquerading as depression.
The point isn’t to label you. It’s to understand you. The treatment that works for major depressive disorder doesn’t work the same for bipolar depression. Precision matters.
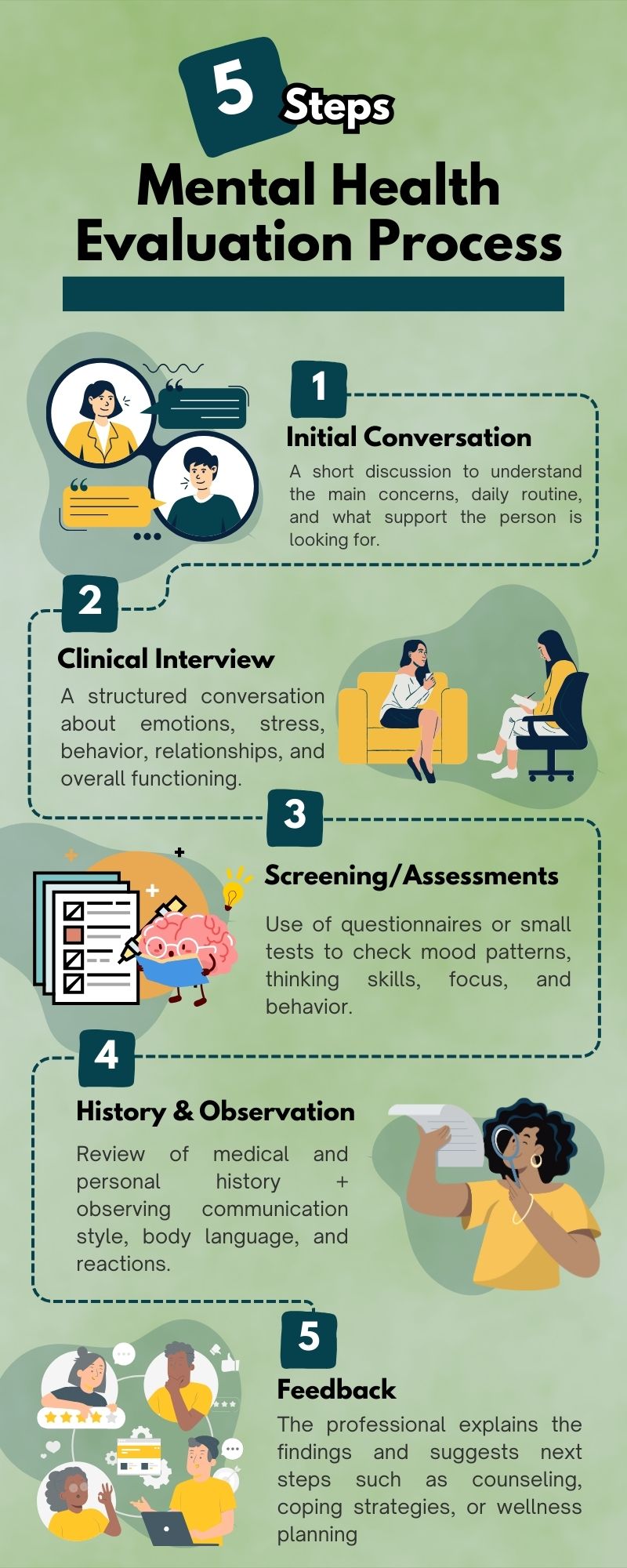
4. Risk Assessment: The Question Nobody Wants to Ask
This makes people dread. The part that makes them consider lying.
“Have you thought about hurting yourself?”
It’s a hard question. Still, it’s not optional.
Risk assessment isn’t about judgment. It’s not about locking you up the second you admit things are dark. It’s about safety. Yours specifically. Your clinician needs to know if you’re thinking about suicide. Not just vaguely. Specifically. Do you have a plan? Have you rehearsed it in your mind?
These aren’t comfortable questions. They’re essential. Do you know what happens when we don’t ask: people die. People who would have lived if someone had just asked the direct question instead of dancing around it.
Therefore, the assessment has to happen. We can’t help you. If we don’t know how close to the edge you’re standing.
5. Psychosocial Assessment: Your Life Beyond Symptoms
Depression doesn’t exist in a vacuum. Neither does anxiety. You don’t just have symptoms. You have a life. A job or the lack of one. Relationships that are holding or fracturing. A place you live that’s either safe or very much not.
This assessment shapes treatment recommendations. Someone with stable housing and strong support has different options than someone who’s homeless and isolated. Both deserve help. But the path looks different.
Final Words
So you’ve been through it all. Talked about your history. Been observed. Filled out forms. Answered hard questions about safety. Described your living situation.
Now the pieces come together into something like clarity. Your clinician takes everything they’ve learned and creates a clinical picture. This is what you’re dealing with. This is why it probably started. This is how it’s affecting you now.
Then comes the plan. Maybe it’s therapy. Maybe it’s medication. Probably it’s both.
At Clover Behavioral Health, we’ve walked hundreds of people through these five components. Those who arrived dispersed and left with at least the outline of a map.
And you are correct; in case you are reading this and wondering, I should probably get evaluated. You do not call the fire department until the house completely burns down. Call us at 978-216-7765. Not because you have to have everything figured out. You don’t. And that’s exactly why we’re here.