When Two Battles Become One: Dual Diagnosis Treatment for Bipolar Disorder in MA
October 1, 2007. Groundbreaking results published in the American Journal of Psychiatry would change the way we treat bipolar disorder and addiction.
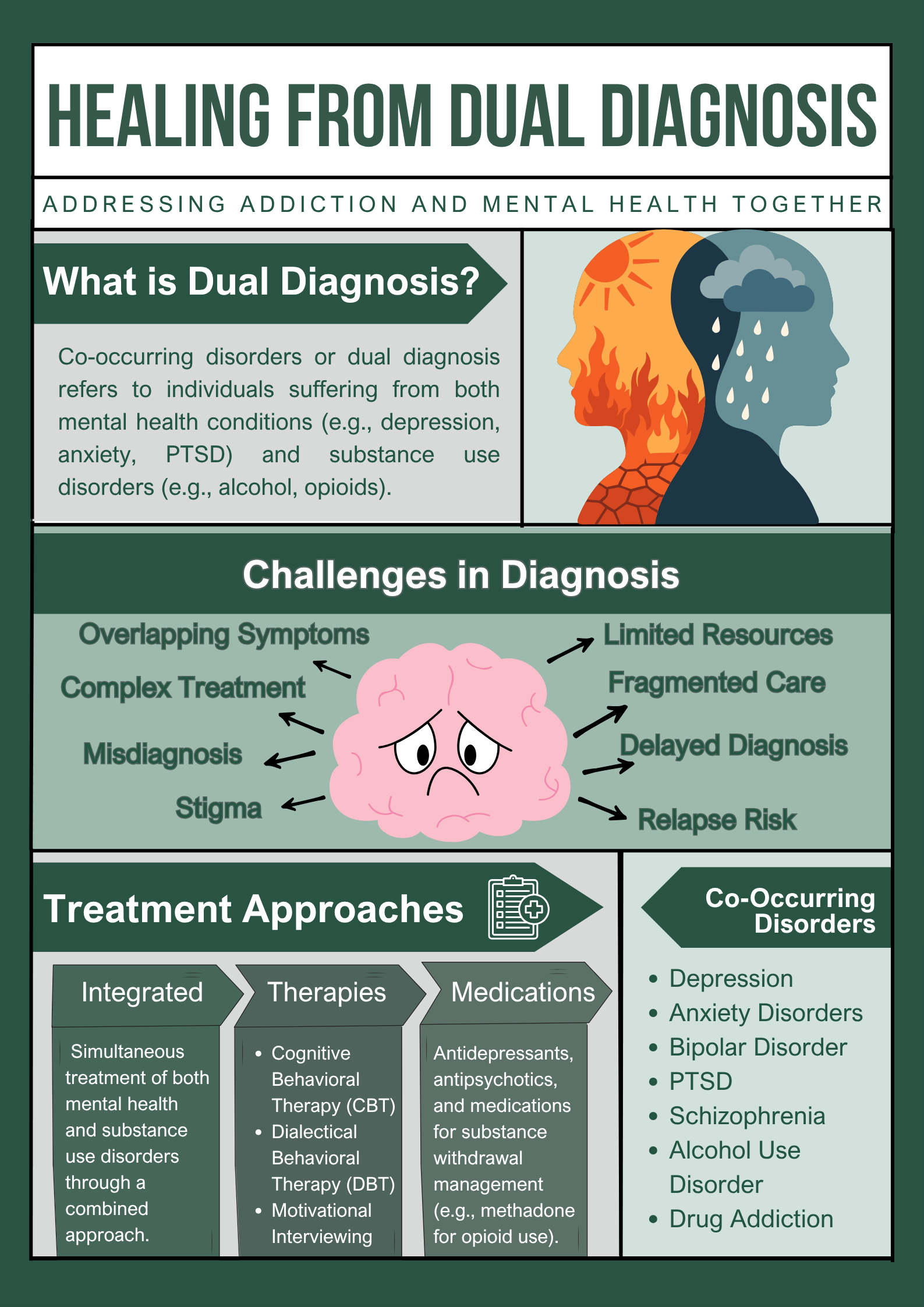
Scientists discovered that concurrent treatment of the two conditions reduced substance use by far in comparison to treating them individually. That fact remains certain almost twenty years later: you cannot wage half a war and hope to succeed in it.
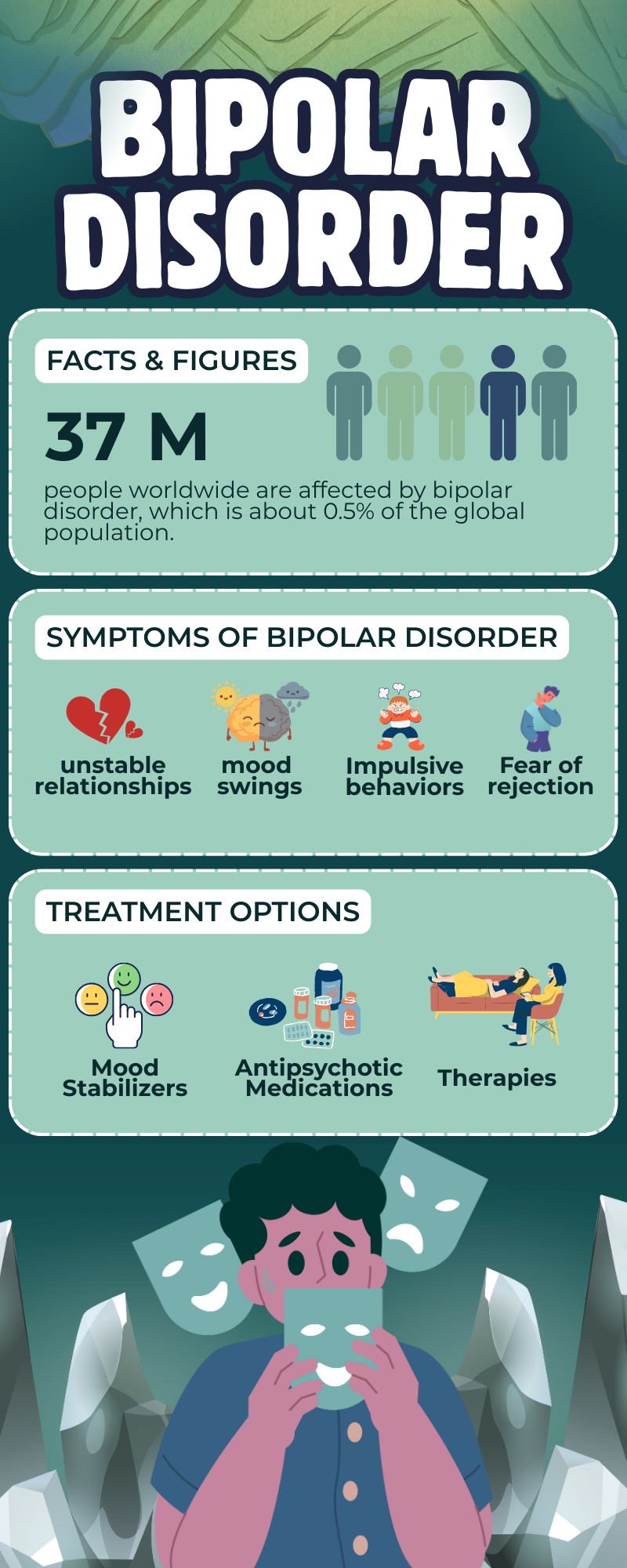
Approximately 60 percent of bipolar disorder patients will become substance abusers at some stage of their lives. Read that again. Is that self-medication? Absolutely. Does it work? Not even close.
The thing is, substances don’t just fail to help. Rather, they actively sabotage. Alcohol disrupts sleep, which triggers episodes. Cocaine mimics or worsens mania. Sedatives intensify the depression. It is a snake that swallows its tail, and amid all the confusion, the person caught in the middle of it is fading.
In Massachusetts, where everyone appears to have it all figured out, this fight happens behind closed doors. Nobody even talks about it. However, at Clover Behavioral Health, we see it. We treat it. And most importantly? We understand it.
Why Bipolar and Addiction Are a Package Deal
The connection isn’t random. During mania, your brain won’t shut up. Thoughts sprint ahead of you. Sleep feels impossible, and honestly, who needs it when you’re this productive? Some people grab alcohol or benzos, trying to slow the spin. Others chase stimulants to keep riding the wave. It starts as a solution. It ends as another problem.
Then depression hits like a freight train. Everything hurts. Getting out of bed feels like lifting cement. And in those moments, substances promise an escape. A few hours where the weight lifts, even if it comes crashing back harder tomorrow.
How Clover Behavioral Health Treats the Whole Fight
We don’t do halfway. When someone walks through our doors struggling with both bipolar disorder and substance use, we see one interconnected challenge. Not two separate problems to tackle one at a time.
Starting With the Full Picture
First, we listen. How long have the mood swings been happening? When did the substance use begin? Are there traumas lurking underneath? Medical complications?
We may need a period of drug and alcohol abstinence to see whether bipolar disorder exists without substance use. This helps us adjust medications and treatment more accurately. Our holistic approach focuses on the root causes, not just the symptoms.
Medication That Works When Substances Are in the Picture
Managing medication for bipolar disorder is already delicate. Add substances into the mix, and it becomes a high-wire act. Lithium and valproate are effective for mood symptoms and may reduce substance use as mood stability improves.
Our psychiatrists specialize in dual diagnosis medication management. They know which mood stabilizers work best during recovery. They understand how substances interfere with medications. And they monitor closely, making adjustments before small issues snowball.
Evidence-Based Therapies Designed for Dual Diagnosis
Integrated Group Therapy (IGT):
This isn’t regular group therapy. IGT works on a principle of conceptualizing both disorders as manifestations of a common underlying process called “bipolar substance abuse.” Instead of treating bipolar in one session and addiction in another, IGT addresses both simultaneously. Research proves it works, as patients receiving integrated group therapy had significantly fewer days of substance use during treatment and follow-up.
The beauty of IGT? You’re sitting with people who understand both struggles. They get what it’s like when racing thoughts meet cravings. When depression whispers that just one drink will help. That shared understanding becomes its own form of healing.
Cognitive Behavioral Therapy (CBT):
We help you identify the thought patterns driving both mood episodes and substance use. What are your triggers? What happens right before you reach for a substance or feel an episode coming? Once you can spot the patterns, you can interrupt them. Build different responses. Healthier coping strategies that work when life gets messy.
Dialectical Behavior Therapy (DBT):
This imparts real-life skills for dealing with strong emotions without resorting to substances. Mindfulness training makes you fully aware of your feelings and thoughts. This awareness creates a gap between emotion and reaction, allowing you to take intentional actions instead of impulsive ones. On the other hand, distress tolerance will provide you with options when you are hit hard by your cravings. DBT also regulates intense emotions to reduce the likelihood of impulsive actions like substance use.
Motivational Enhancement Therapy (MET):
It is useful in treating bipolar disorder, particularly when combined with treatment and medication. It aims to boost internal motivation and change harmful behaviors through a structured approach. Our licensed psychologists use a client-centered strategy where each individual is motivated to find their own reasons for change. Instead of telling you what to do, we equip you with skills to figure out solutions yourself.
Flexible Care That Moves With You
Recovery isn’t linear. Some days you’ll feel solid. Other days you’ll need more support. That’s why we offer different levels of care:
Partial Hospitalization Program (PHP):
Daily treatment, but not 24-hour hospitalization. Ideal in initial stages when the two conditions require urgent concerted efforts.
Intensive Outpatient Program (IOP):
It gives you the ability to continue with work or family life and get considerable assistance a few times a week. Sufficient structure to keep the momentum going without halting your whole life.
Outpatient Care:
The treatment offered to individuals that have achieved a stable state yet require additional assistance includes individual therapy, group sessions, and medication management.
The beauty? You are able to step up or down depending on what you need today, not three months ago.
Final Words
Clover Behavioral Health takes in most major insurance plans – such as Multiplan, Horizon, Beacon, Empire, Meritain, and UMR. So, money is no longer the reason to deprive yourself of care that would transform your life.
Give us a call at 978-216-7765 and talk to a person who can relate to what you are going through. We will give you the answers to the questions, clarify your choices, and assist with the first step to the treatment of both conditions.